The Warning Sign You Can See
I want you to do something for me. Stand up and look at yourself sideways in a mirror.
Does your belly stick out more than it used to? Not just a little—really protrude?
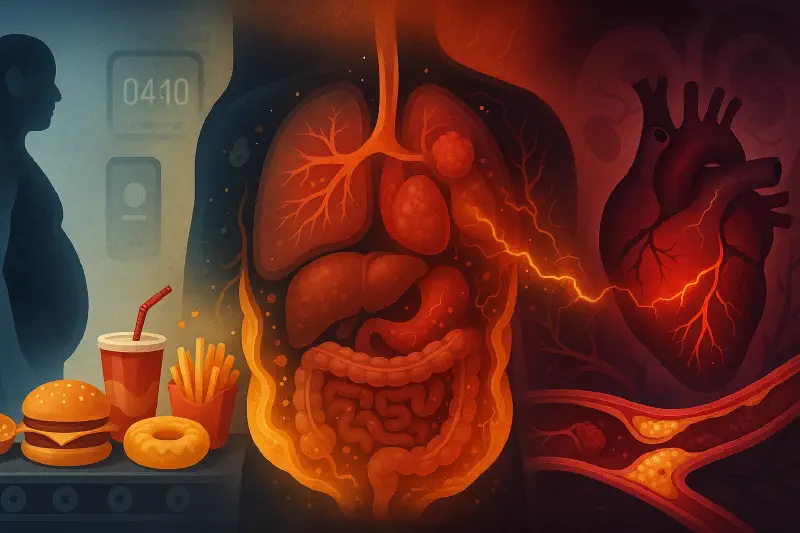
If the answer is yes, I have news that might unsettle you: that’s not just weight gain. That visible change is a window into something happening deep inside your body, something that’s silently setting the stage for heart disease, diabetes, and systemic inflammation.
That fat isn’t like the fat on your thighs or arms. It’s called visceral fat, and it behaves completely differently. It wraps around your liver, your pancreas, your heart. And unlike the subcutaneous fat you can pinch, visceral fat is metabolically active—meaning it’s constantly producing inflammatory compounds that spread throughout your entire body.
But here’s what really matters: visceral fat is a symptom, not the root cause. To understand what’s really happening, we need to talk about insulin.
The Glucose Problem: Why Your Body Needs Insulin
Let me start with something that surprised me when I first learned it: glucose is toxic.
I don’t mean toxic in the way arsenic is toxic, where a tiny amount kills you. I mean that glucose floating freely in your bloodstream damages things. It’s called glycation—glucose molecules attach themselves to proteins in your blood, to the walls of your blood vessels, to your hemoglobin. Once a molecule gets glycated, it can’t work properly anymore. Your enzymes malfunction. Your hormones don’t signal correctly. Your tissues age prematurely.
This is why your body treats rising blood sugar as an emergency.
Here’s the elegant system your body designed to handle this: When you eat—especially foods containing carbohydrates or sugar—your digestive system breaks them down into glucose. That glucose enters your bloodstream. Your pancreas, always monitoring your blood, detects the glucose spike and releases insulin.
Think of insulin as a delivery driver. Its job is to escort glucose out of your bloodstream and into your cells—your muscles, your liver, your organs—where it can be used for energy or stored for later use. Once insulin completes its delivery route, glucose levels drop back to baseline, insulin levels fall, and everything returns to normal.
When you eat occasionally—say, two or three times a day with hours between meals—this system works beautifully.
How Constant Eating Breaks Everything
But that’s not how we eat anymore.
We eat breakfast. We snack mid-morning. We have lunch. We snack mid-afternoon. We eat dinner. We snack in the evening. We’re drinking sugary coffee drinks, sodas, fruit juices throughout the day. We’re consuming processed foods engineered to be quickly absorbed—foods stripped of fiber specifically so they’ll spike our blood sugar faster.
What does this mean for your body?
Your pancreas keeps releasing insulin. Again. And again. And again. Insulin never really gets a break. And here’s where the problem begins: when a hormone stays elevated in your body for extended periods, your cells start to become less responsive to it.
It’s like living next to a train track. At first, every train that passes demands your attention—you hear it, you feel it, you react. But after months of constant trains, your brain tunes themout. You barely notice them anymore. Your cells do the same thing with insulin.
This is insulin resistance—when your cells stop responding effectively to insulin’s signal.
But your blood sugar still needs to come down. So your pancreas compensates by producing even more insulin. More and more insulin floods into your bloodstream just to accomplish what a small amount used to do.
And this is where the real damage begins.
The Cascade: From High Insulin to Visceral Fat
Insulin isn’t just a delivery driver for glucose. It’s also a storage hormone—one of the most powerful ones in your body.
When insulin levels are high, your body receives one clear message: store energy, don’t burn it. High insulin essentially locks your fat cells. You can’t access stored fat for energy while insulin is elevated. You can only store more.
But it gets worse than that.
When insulin is chronically elevated—which happens with insulin resistance—your body doesn’t just store fat randomly. It stores it preferentially as visceral fat around your midsection and organs.
Let me explain why this happens. When you eat carbohydrates and sugar frequently, glucose floods into your liver. Your liver converts that glucose into fat through a process called de novo lipogenesis—literally, “making new fat.” That newly created fat accumulates around your liver first (fatty liver disease), then spreads to your pancreas and around your heart and other organs.
This is a fundamentally different process than gaining weight from eating too many calories overall. If you ate 3,000 calories of mixed foods—protein, fats, vegetables—you’d gain weight everywhere: your arms, legs, face, everywhere roughly proportionally.
But if you eat glucose and trigger constant insulin spikes? Your belly protrudes while the rest of you stays relatively normal. That’s the phenotype—the visible characteristic—of someone with hyperinsulinemia (chronically high insulin).
And here’s what makes this truly dangerous: visceral fat isn’t inert.
Why Visceral Fat Is Uniquely Harmful
If I took a biopsy of the fat on your buttocks and compared it to a biopsy of the visceral fat in your belly, I’d see two completely different tissues under the microscope.
The subcutaneous fat—the kind you can pinch—is relatively quiet metabolically. It stores energy. That’s about it.
Visceral fat is a different beast entirely. It’s packed with immune cells and it’s actively producing inflammatory molecules: interleukin-6, tumor necrosis factor-alpha, C-reactive protein. These are the same inflammatory markers we see elevated in people with autoimmune diseases, chronic infections, and cancer.
Why does visceral fat produce these molecules? Because your body recognizes something is wrong. Visceral fat shouldn’t be there in those quantities. Your immune system is reacting to it as if it’s a foreign invader.
So now you have this fat depot sitting inside your abdomen, constantly pumping inflammatory compounds into your bloodstream. These compounds travel everywhere—to your brain, your heart, your blood vessels, your joints, your gut.
This is systemic inflammation. And systemic inflammation is the foundation of nearly every chronic disease we face.
The Gut Connection: When Your Borders Fail
Let me add another layer that caught me off guard when I first learned about it.
Your gut—your intestinal lining—is supposed to be the most carefully guarded border in your body. It’s where the outside world (the food you eat, the bacteria in your intestines) meets your inside world (your bloodstream, your immune system).
When your gut microbiome is healthy—when you have the right balance of bacteria—those bacteria produce compounds that maintain the integrity of your intestinal wall. The cells lining your gut fit together tightly, like a well-sealed barrier.
But when your microbiome becomes dysfunctional—often because of the same processed foods, lack of fiber, and constant eating that drives insulin resistance—the tight junctions between intestinal cells start to loosen.
This is called “leaky gut.” And when your gut becomes leaky, molecules that should stay inside your intestines—dead bacterial cell wall fragments called lipopolysaccharides—slip through into your bloodstream.
Where do they go first? Straight to your liver through the portal vein.
Your liver tries to deal with this invasion, but it gets overwhelmed. This adds to the inflammation. It worsens the fatty liver. It creates more insulin resistance. The whole system spirals.
So now you have multiple sources of inflammation: the visceral fat producing inflammatory compounds, and your leaky gut allowing bacterial products into your bloodstream.
Your body is under siege from the inside.
The Perfect Storm: Three Pathways to Heart Disease
Now we get to the heart of the matter—literally.
Heart disease is the number one cause of death worldwide. And what we’ve just described—insulin resistance, visceral fat, inflammation, leaky gut—creates a perfect storm that attacks your cardiovascular system through three separate mechanisms:
Pathway 1: Plaque Formation
Your arteries aren’t just pipes. The inner lining—called the endothelium—is a living, active tissue that regulates blood flow, prevents clotting, and repairs damage.
When inflammatory molecules circulate in your bloodstream, they damage this endothelial lining. Your body tries to repair the damage. It sends cholesterol particles (specifically, LDL particles) to patch the injured areas. But when those LDL particles themselves become damaged—oxidized and transformed into small, dense particles because of the inflammation, high glucose, and other toxins—they get stuck in the artery wall.
Your immune system sees these stuck, damaged LDL particles and sends white blood cells called macrophages to clean them up. The macrophages engulf the damaged LDL, but they can’t properly break it down. They become engorged—turning into what we call “foam cells”—and they get stuck in the artery wall too.
This accumulation becomes a plaque. Think of it like a pimple forming on the inside of your artery. It’s a buildup of inflammatory cells, damaged cholesterol, and fibrous tissue.
And you’re making more and more of these plaques throughout your entire arterial system.
Pathway 2: Plaque Instability
Plaques themselves don’t usually cause heart attacks. A stable plaque—even one that’s partially blocking an artery—can sit there for years without killing you. You might get chest pain when you exercise (because blood flow is restricted), but you won’t necessarily have a heart attack.
A heart attack happens when a plaque ruptures—when that pimple on the inside of your artery bursts open.
What causes rupture? Inflammation.
When you have chronic, systemic inflammation—the kind driven by visceral fat and insulin resistance—that inflammation destabilizes your plaques. It weakens the fibrous cap holding the plaque together. And one day, often triggered by a spike in inflammation or blood pressure, the plaque cracks open.
When a plaque ruptures, it exposes the raw, inflamed tissue beneath. And this triggers the third pathway.
Pathway 3: Blood Clot Formation
Your blood is always ready to form clots. It has to be—otherwise, any cut would make you bleed to death. When your blood detects exposed tissue (like a ruptured plaque), clotting factors activate immediately.
Under normal circumstances, this is helpful. But when you have chronic inflammation—which you do with insulin resistance—your blood is hypercoagulable. That means it’s primed to clot more easily and more aggressively.
So when that plaque ruptures, a massive blood clot forms on top of it. The clot completely blocks the artery. No blood flows past that point. The heart muscle downstream from the blockage is starved of oxygen.
That’s a heart attack.
And here’s the truly frightening part: this can happen even in relatively young arteries, even in people who think they’re healthy, because the underlying driver—insulin resistance and inflammation—has been silently building for years.
Dr. Praip Jamnadas, a cardiologist who’s treated over 30,000 patients, has seen this exact cascade in a 28-year-old. Twenty-eight. That patient wasn’t diabetic. His blood sugar levels looked fine on standard tests. But he had visceral fat, he had a fatty liver, and when Dr. Jamnadas measured his insulin levels, they were sky-high.
He had been insulin resistant for years without knowing it. And it gave him a heart attack at 28.
Beyond the Heart: The Whole-Body Impact
I need to emphasize something: while heart disease is the most dramatic outcome of this process, the damage spreads everywhere.
Your brain suffers. Inflammation crosses the blood-brain barrier. Depression isn’t purely psychological—research increasingly shows that depression is inflammation in the brain. The mental fog, memory problems, and mood disturbances people experience aren’t character flaws. They’re inflammatory symptoms.
Your pancreas deteriorates. The very organ producing all that extra insulin is being damaged by the insulin it’s making. Eventually, after years of overwork, it starts to fail. Beta cells—the insulin-producing cells—burn out. This is when you transition from insulin resistance (high insulin, normal blood sugar) to type 2 diabetes (damaged pancreas, high blood sugar). By that point, you’ve often already developed cardiovascular disease.
Your microcirculation fails. It’s not just the large arteries forming plaques. The tiny capillaries—the smallest blood vessels that actually deliver oxygen and nutrients to your tissues—become dysfunctional. When your capillaries don’t work properly, every organ suffers. Your kidneys filter less effectively. Your eyes develop vision problems. Your nerves start to malfunction (diabetic neuropathy). Your skin doesn’t heal well.
Your joints hurt. That chronic inflammation affects your joints. People assume joint pain is just “wear and tear” or “getting older.” But many people with insulin resistance see their joint pain dramatically improve when they reduce inflammation—because it was never purely mechanical damage.
Your immune system gets confused. Chronic inflammation can trigger autoimmune responses. Your body, constantly on high alert, starts attacking its own tissues. Rheumatoid arthritis, psoriasis, inflammatory bowel disease—these conditions are all far more common in people with metabolic dysfunction.
This is why I said at the beginning: that protruding belly isn’t just a cosmetic concern. It’s a visible manifestation of a systemic problem affecting nearly every system in your body.
The Modern Epidemic: Why This Is Getting Worse
For most of human history, this wasn’t a problem.
Our ancestors didn’t have access to food 24/7. They ate when food was available, and then they went hours—sometimes days—without eating. During those fasting periods, insulin levels dropped. The body shifted from “storage mode” to “burning mode.” After about 12 hours without food, the body starts pulling energy from fat stores. And the first fat it mobilizes? Visceral fat.
This natural cycling between fed and fasted states kept insulin levels in check. It prevented insulin resistance from developing. It gave the pancreas regular breaks. It allowed the body to burn off visceral fat before it accumulated to dangerous levels.
But with modern industrialized food systems, we’ve completely lost this physiology.
We wake up and eat breakfast—often high-carb cereal, toast, orange juice, all of which spike insulin. We snack mid-morning. We eat lunch. We snack mid-afternoon. We eat dinner. We snack in the evening, maybe some ice cream or chips while watching TV.
Insulin never drops. We never enter the fasted state. We never give our bodies the signal to burn fat.
On top of that, we’re eating processed foods specifically engineered to be rapidly absorbed. Food manufacturers remove fiber because it extends shelf life and creates more consistent texture. But fiber is what slows glucose absorption. Without it, we get massive insulin spikes.
We’re drinking our calories—sodas, lattes, fruit juices, energy drinks—which spike insulin even faster than solid food.
We’re eating foods loaded with industrial seed oils (vegetable oils, canola oil, soybean oil), which are extremely high in omega-6 fatty acids. These oils promote inflammation and oxidative stress, making our LDL particles more likely to become the small, dense, damaged kind that form plaques.
We’re exposed to more toxins—pesticides, herbicides, plastics, mold, heavy metals—than ever before. These toxins disrupt our metabolism, damage our gut bacteria, and add to the inflammatory burden.
We’re sleeping less. Even one night of poor sleep makes you insulin resistant the next day.
We’re chronically stressed, which keeps cortisol elevated, which worsens insulin resistance.
It’s not just one thing. It’s the entire environment of modern living conspiring to break our metabolic health.
And the result? We’re seeing an epidemic of insulin resistance, metabolic syndrome, type 2 diabetes, and cardiovascular disease—at younger and younger ages.
Cardiologists used to treat mostly patients over 65. Now, about half of heart disease cases occur in people under 65. And it’s not rare anymore to see patients in their 30s and 40s having heart attacks.
This is the canary in the coal mine. This is your body’s early warning system screaming at you that something is fundamentally wrong.
The Silent Years: Why You Don’t Feel It Until It’s Advanced
Here’s what makes insulin resistance so insidious: you can have it for years—even a decade—without knowing.
Your fasting blood sugar looks fine on standard tests. Your doctor says, “You’re not diabetic, everything’s normal.” But underneath, your insulin is three times higher than it should be. You’re accumulating visceral fat. Your liver is getting fatty. Inflammation is rising. Plaques are forming in your arteries.
All of this is happening silently.
By the time your blood sugar finally rises enough to trigger a diabetes diagnosis, you’ve already had years of damage. You likely already have coronary artery disease. You’ve already lost significant beta cell function in your pancreas. You’ve already built up substantial visceral fat.
This is why waiting for symptoms—or waiting for standard tests to show problems—is a terrible strategy.
The belly fat is actually one of the few visible early warning signs you get. If you see it, you should act on it.
What We’ve Learned: The Chain of Events
Let me pull this all together into a clear sequence, because understanding this chain is crucial:
Step 1: Frequent eating and processed foods → You consume carbohydrates and sugars multiple times throughout the day, every day.
Step 2: Chronic insulin elevation → Your pancreas releases insulin repeatedly. Insulin levels stay elevated for most of your waking hours.
Step 3: Insulin resistance develops → Your cells become less responsive to insulin. Your pancreas compensates by producing even more insulin.
Step 4: Visceral fat accumulates → High insulin drives fat storage, particularly around your organs. Glucose is converted to fat in your liver.
Step 5: Inflammation rises → Visceral fat produces inflammatory compounds. A leaky gut (often caused by poor diet and microbiome dysfunction) allows bacterial products into your bloodstream, adding more inflammation.
Step 6: Cardiovascular damage begins → Inflammation damages your arteries. Damaged LDL particles form plaques. Plaques become unstable. Your blood becomes more prone to clotting.
Step 7: Whole-body deterioration → The same inflammation affects your brain (mood, cognition), your pancreas (eventual diabetes), your joints (pain), your microcirculation (organ dysfunction), and your immune system (autoimmune risk).
Step 8: Acute events → A plaque ruptures. A clot forms. You have a heart attack. Or your pancreas finally gives out and you develop diabetes. Or you develop an autoimmune condition. These acute events are the endpoint of years of silent progression.
This is the mechanism. This is what insulin resistance actually is and what it does to your body.
The Crucial Distinction: Correlation vs. Causation
Before we close, I want to address something important: some of you might be thinking, “But I know people who eat terribly and don’t have problems,” or “I know thin people who had heart attacks.”
Yes. Biology isn’t deterministic. There’s individual variation.
Some people have genetics that protect them—at least for a while. Some people have more resilient insulin signaling. Some people have better antioxidant systems that protect their LDL from oxidation. Some people have robust gut microbiomes despite poor diets.
But those are exceptions, not the rule. And even those people are often accumulating damage—they just haven’t crossed the threshold into disease yet.
On the flip side, you can be thin and still have insulin resistance if your fat is preferentially stored as visceral fat. You can have a normal BMI and still have a fatty liver, high insulin, and inflammation.
The point isn’t that insulin resistance guarantees heart disease in everyone. The point is that it dramatically increases your risk, and it’s the underlying mechanism for the vast majority of cardiovascular disease cases we see today.
Where Do We Go From Here?
So now you understand the mechanism. You understand what’s happening inside your body when insulin resistance develops. You understand the cascade from constant eating → high insulin → visceral fat → inflammation → cardiovascular disease.
You understand why that belly fat is a warning sign.
And most importantly, you understand that this isn’t random. This isn’t just bad luck or bad genetics. This is a logical, predictable consequence of how we’re eating and living in the modern world.
But here’s the critical part I want you to remember: this is reversible.
Every step in this cascade can be interrupted. Visceral fat can be mobilized and burned. Inflammation can be reduced. Insulin sensitivity can be restored. Plaque progression can be slowed or even halted. Your gut microbiome can be repaired. Your metabolic health can be rebuilt.
In the next post, we’ll talk about exactly how to do that. We’ll cover fasting protocols, dietary changes, specific exercises, supplements, testing you should request from your doctor, and lifestyle factors like sleep and stress management.
But I wanted you to understand the “what” and the “why” first. Because when you understand the mechanism—when you really grasp what’s happening inside your body—the solutions make sense. They’re not random rules or fad diets. They’re logical interventions targeting specific parts of the cascade we just mapped out.
Your body is an incredibly sophisticated system. When you give it the right conditions, it wants to heal. It wants to return to balance.
You just need to understand what those conditions are.
Key Takeaways:
- Insulin resistance develops when chronically elevated insulin makes your cells less responsive, forcing your pancreas to produce even more insulin
- High insulin drives visceral fat accumulation, which actively produces inflammatory compounds
- Inflammation damages your arteries, destabilizes plaques, and makes your blood more prone to clotting—creating the perfect storm for heart attacks
- The same inflammatory cascade damages your brain, pancreas, joints, microcirculation, and immune system
- Modern eating patterns (frequent meals, processed foods, sugar) keep insulin elevated and prevent the natural fasting state that would burn visceral fat
- This process is often silent for years—you can have severe insulin resistance while standard blood tests still show “normal” results
- The visible warning sign: a protruding belly with fat concentrated around your midsection
- Most importantly: this entire cascade is reversible with the right interventions
(Written by Human, improved using AI where applicable.)